In 2019, when my father was in the Intensive Care Unit of one of Nigeria’s biggest tertiary hospitals in the Federal Capital Territory, one of the most contentious issues my family experienced was the constant chasing after specialist doctors to assess him and answer our burning questions. We would wait hours for the single cardiologist on call to go through several wards before coming to his bedside, often tired from seeing more patients than he should. On some days, there was just no cardiologist to assess my father who had a severe heart condition. This is the reality of several Nigerians, where people wait several hours and sometimes days to see a doctor and often more when it is a specialist. This has now become the norm and easily one of the situations under Nigeria’s Manage It Like That (MILT) story.
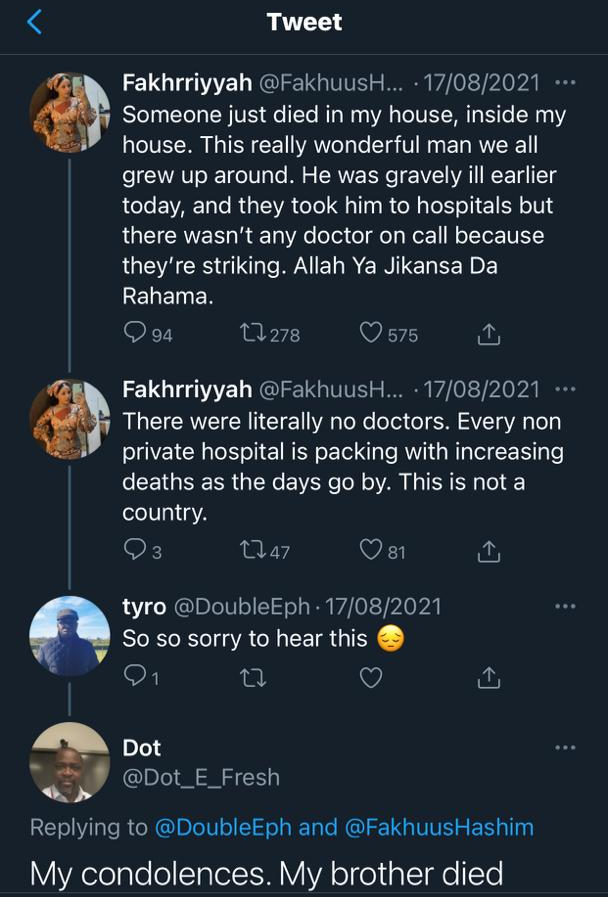
In the last two weeks, I have read with horror the experiences of Nigerians affected by the ongoing medical doctors’ strike. People have reported watching their loved ones die because they could not access a doctor. The impact of the ongoing strike is arguably underreported, possibly because the public is distracted by the third wave of the COVID-19 pandemic or the political football that discussions with stakeholders has degenerated into. The penchant for the Nigerian media is to focus on the more sensational stories over highlighting the more salient issues. There is also the fact that Nigerians have “bigger” problems to ponder over like the next meal, a job after school, incessant kidnappings and loss of lives. Nonetheless, there is no doubt that we are sitting on a ticking time bomb — the growing shortage of medical doctors.
The shortage of medical doctors has been a historical challenge for Nigeria. For decades, our very best have left the nation’s shores for greener pastures and better job opportunities. There is no doubt that the poor quality of health care in Nigeria is related in large part, to the critical shortage of health care workers among other factors. In the context of the COVID-19 pandemic, annual large outbreaks of infectious diseases and an exploding population density, this critical issue must be treated as a state of emergency. It should be receiving the highest level of political attention, media spotlight and advocacy for a better health sector.

Are Our Medical Doctors Truly in Excess Supply?
In April 2019, the Minister of Labour, Dr. Chris Ngige, who is also a Medical Doctor, stated that Nigeria is not lacking medical doctors. In his words: “We have surplus. If you have surplus, you export.” This is however, far from the truth. In 2016, the World Health Organisation identified that countries should aim for a minimum of 4.45 medical doctors, nurses and midwives per 1,000 population. According to World Bank data, latest figures from 2018 show that Nigeria has 0.381 medical doctors per 1,000 people, meaning, for every 10,000 Nigerians, there are about three medical doctors available. In a country with some of the worst health indices, this is grossly insufficient and unacceptable.
In 2018, NOI Polls and Nigeria Health Watch produced a survey report on the Emigration of Nigerian Medical Doctors where findings indicate that the United Kingdom is the leading country for medical doctors seeking opportunities, with 93% of the survey population interested in emigrating to that country. This is followed by the United States of America with 86%, Canada, Saudi Arabia and Australia rounding up the top 5 countries with 60%, 59% and 52% respectively.
This begs the question of how Nigeria is “comfortable” with losing its brightest talents, with its population of just over 200 million people , the poor socio-economic indicators and high prevalence of infectious diseases, to countries like the United Kingdom, Canada and Saudi Arabia with populations of 66 million, 37 million, and 34 million respectively.

Declaring a State of Emergency
It is no longer news that countries actively recruit medical doctors from Nigeria. This has gone on for decades. However, in recent years, it has steadily climbed to a brazen level. We have seen videos of officials from the Saudi Arabian government organising recruitment exercises for Nigerian medical doctors in Lagos and Abuja. This ongoing recruitment may not only be described as unethical but arguably goes against the Global Code of Practice on the International Recruitment of Health Personnel which unequivocally states in Article 3, Section 4, that “Member States should take into account the right to the highest attainable standard of health of the populations of source countries, individual rights of health personnel to leave any country in accordance with applicable laws, in order to mitigate the negative effects and maximise the positive effects of migration on the health systems of the source countries.”
At what point will the federal government and national authorities realise that Nigeria is on the brink of a national health disaster if we continue to lose our medical doctors and not address the grievances contributing to their emigration? Will the long wait for medical doctors and strike actions every other quarter of the year become a MILT situation? The health sector has fallen to a state of complete disarray; a state of emergency is imminent, and we must not lose this opportunity.
Where Do We Go from Here? -Recommendations for a Sufficient, Present and Active Health Care Workforce
There is no doubt that countries like Nigeria compete with the best institutions in the world for quality manpower. The brain drain will happen, however, how can we mitigate issues such as low salaries of health care workers in the public health sector? This could be addressed by permitting health professionals in the public sector to do some private practice through a much better regulated and accountable approach; providing educational benefits for their children, substantial welfare and protection packages for health care workers to work in rural and hard-to-reach communities. Treating the brain drain as a national health emergency, and instituting measures to address this, is key to reducing the emigration of the health workforce.
According to a World Bank article, we must first recognise that persistent emigration is usually the symptom of an underlying problem. Economic incentives are usually a major reason for labour migrations, so, making salaries and welfare benefits more competitive, would entice Nigeria’s medical doctors and health care workers to remain. Ultimately, the most effective long-term approach that Nigeria can adopt to truncate this brain drain is to limit the “push factors” that drive medical doctors to leave the country in the first place– this means providing better career opportunities, improving working conditions and remuneration and creating an environment where better opportunities, enable a better standard of living.
The rising insecurity in our country has several implications and one of the least recognised is the emigration of our best talents including medical doctors. We need to make Nigeria safer not just for the present, but to avert future disasters.
Addressing the root causes of strike actions — poor remuneration, bad working conditions, poor welfare packages, inadequate incentives, lack of funding of health facilities, poor conditions of health facilities and limited career structures — is key to putting an end to the brain drain. The question is, are the Nigerian authorities ready to keep our own at home?



I wish to comment on your referring to the hiring practices of foreign governments in Nigeria as unethical. Are you aware of how many qualified doctors are waiting for residency training places? Do you know how many specialists cannot get jobs where they can practice their skills? Do you know the pittance some private clinics pay qualified doctors? To discourage emigration of doctors is to condemn many to slavery. If Nigeria can find money to pay legislators and oil workers those humongous salaries, they should find money to pay doctors. If indeed they value the life of the average Nigerian.
When you have a country where the Janjaweeds from Futa Jallon claim that God has given them Nigeria for their eternal inheritance and that by all foul means they are going to drive all the owners of the place away so that they can occupy the place completely, why do you think that these measures by them and their collaborators, which is doing exactly what they have objectively planned to do, will be addressed otherwise? Please let nobody continue to deceive themselves on these matters at hand! We will better do what we ALL need to do CORPORATELY to arrest the nonsense, or we simply run away too, OR keep our mouths shut!
Working in the very epicentre of this fast developing epidemic of the brain drain, I have wracked my brain to come up with some strategies that can be applied. I have often imagined several “what if” moments where I have a magic wand, unlimited resources and a willing cabinet of people as thinkers and doers… What indeed will it take to strengthen our health system? One thing is for sure, if we all had no choice but to use this health system, we would work to improve it. We need to stop all government political holders from accessing healthcare in the UAE, UK, US and other popular medical tourist spots
To me, the authorities appear not to know what to do or appreciate the enormity of the health workforce problem. This is an emergency situation. It is a reflection of my belief that countries which value the lives of their people make health a priority. This is not the case here. The system requires a total overhaul.