Most mothers look forward to a lifetime of giving their offspring gifts, beginning with the gift of life. Imagine the devastation that some face when they realise that they could pass on a lifelong illness to their precious little one, due to factors beyond their control. This is often the reality of a pregnant woman who is HIV positive.
Tari (not real name) was in shock when she learnt she was HIV positive at her 3-month antenatal visit. She could not believe the results because she got tested often.
For Dunni, her test results coming back positive for HIV had an immediate mental effect on her. “I nearly died. When I left the hospital, I thought of involving myself in an accident just to end it all. When I got on to the expressway, I stood in the middle waiting for any vehicle to crush me. Until a passer-by pushed me out of the road,” she said.
An Island of hope for positive mothers
Mother to child transmission of HIV (MTCT) is the transmission of HIV from a HIV-positive mother to her child during pregnancy, labour, delivery or breastfeeding. Without intervention, transmission rates from mother to child range from 15% to 45%. This risk can be reduced to below 5% with effective interventions delivered during pregnancy, labour, delivery and breastfeeding. These interventions primarily involve antiretroviral treatment for the mother and a short course of antiretrovirals for the baby. They also include measures such as testing and counselling, ARVs for the mother and safe childbirth practices to prevent HIV acquisition in the pregnant woman and appropriate breastfeeding practices.
Prevention of mother-to-child transmission (PMTCT) programmes offer a range of services for women of reproductive age living with or at risk of HIV to maintain their health and stop their infants from acquiring HIV.

In 2014, we wrote about the Obio Cottage Hospital in Rivers State and how it was becoming an island of hope for healthcare in Nigeria using their community health insurance model to deliver good quality, affordable care. Recently we returned to the hospital and it seems to have only got better with age. The community people call it a maternity hospital, and walking through the hallways, one could not help but notice the unusually large number of children running around and pregnant mothers waddling behind.
Obio Cottage Hospital (OCH) has a busy antenatal clinic due largely to the Obio Community Health Insurance Scheme model being run by a unique people-public-private partnership which is part of the social investment program of Shell Petroleum Development Company of Nigeria Limited (SPDC) and its joint Venture (JV) partners, the Rivers State Government and the people of Obio community. Dr Chidozie Umejiego, Chief Medical Director (CMD) of OCH, said, “We have more than 200 antenatal patients; including more than 100 outpatients and more than 100 children for immunisation.” Preventing Mother to Child Transmission of HIV is a big part of the antenatal services at Obio. The goal is to make sure that transmission is prevented in 100% of HIV positive pregnant women who present at the facility.
The Community Health Insurance Scheme means that more women come in for antenatal care, more people are tested and the number of new infections identified through case finding for HIV positive pregnant women is high. On average, the hospital tests about 300 women a month compared to 20–50 in facilities where payment of antenatal services is out of pocket, according to Dr Chidozie Umejiego, the Chief Medical Director (CMD) of OCH.
Comprehensive testing
For Aderonke Ojeniyi, Monitoring and Evaluation Officer at OCH, the busier the antenatal clinic, the better for the PMTCT program. Obio runs a robust patient-centred test-all policy for HIV where every client that presents at the facility is offered the opportunity to get tested for HIV but not to the detriment of patients’ rights and ethics. Clients are made aware of the test, are counselled, and only when they accept is the test done. The clinic has not had a case of a client turning down a HIV test, says Aderonke.
Aderonke who doubles as the PMTCT officer at the hospital explains the HIV testing structure; “We have a testing point at the general OPD, then we also have a testing point at the family planning unit, and also at immunisation. Then we also have other points like the INDEX testing at our antenatal clinics, we also do re-testing for pregnant women, within 32 to 36 weeks; then at labour and delivery we offer HIV testing. After the test, if any pregnant woman is positive, she is referred to the counselling unit.”
Counselling
Counselling is a big part of OCH’s PMTCT program. The components of their counselling follow international best practices and include; pre-test counselling of the patient to undergo HIV testing which is intended to provide information about HIV and PMTCT. This is usually done as group counselling for all the women. Here they learn about what to do when a person contracts HIV and how to prevent their children from contracting it. At this point, it is all general information, but it is important groundwork for those whose results may turn out positive.
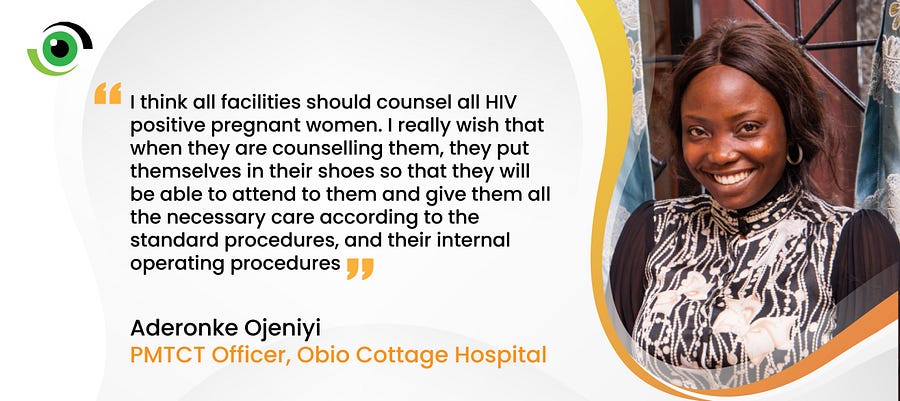
HIV positive clients get special care here. They are discreetly taken to the counselling unit and given an additional refresher course from the morning’s group counselling session. When they understand the basics about HIV and how to live with it, their test result is disclosed to them. At this point, Aderonke says they “give them some time to actually get it, think about it. They would be hurt, we try to reassure them; for those that would cry, we give them time to cry, but later we call them and talk to them again. Then we develop a plan to move forward with them.”
Follow-up counselling and referral is done continuously throughout the pregnancy and beyond, to offer emotional support, HIV prevention and infant-feeding counselling, testing services for partners, and referral to counselling, additional care and treatment services as needed. The immediate worry of most pregnant women who are diagnosed with HIV is the fear of passing it on to their unborn child and often counsellors address this fear and reassure them. With assurance that a positive HIV result is not the end of the world and that there is still a chance for them to deliver and nurture a HIV negative baby, mothers are inspired to follow the careful instructions of healthcare workers under the PMTCT program.
Part of the counselling strategy is guiding the HIV positive client through partner disclosure. They develop plans based on the needs of the client, depending on whether the client can tell her spouse on her own or needs the support of the clinic. “With the help of Madam Ronke, we broke the news to my husband in a way he would not feel bad because before, whenever we heard about somebody being HIV positive, we used to think that it is the end of the person’s life. So she counselled my husband and he saw that I can still give birth to the baby I was carrying, and the child will be HIV negative at birth.” Isoken (not real name), a client at the PMTCT clinic said.
Confidentiality
Stigma remains a big hindrance to successful PMTCT and HIV programs. Obio’s PMTCT program fights stigma and discrimination with confidentiality. The PMTCT counselling unit is cloaked in discretion to ensure that clients who need the services do not turn away in fear. The unit doubles as the M&E unit so that if you walk in, you’d see a lot of charts and graphs, but nothing indicating the real purpose of the room. “Then when somebody tests positive at any point, we try as much as possible to be discreet about the movement of the folder. Patient confidentiality is one of our topmost priorities here.” Aderonke said.
Support Groups and Mentor Mothers
Mentor Mothers are HIV-positive women who serve as peer counsellors for PMTCT clients, providing guidance and support in keeping appointments, promoting antiretroviral adherence, and retention-in-care.
Obio Cottage Hospital’s Mentor Mother programme started in 2016 and strengthens the support groups meetings for HIV positive pregnant women. The PMTCT mentor mother program in Obio Cottage Hospital is implemented by the Institute of Human Virology Nigeria (IHVN) in collaboration with Rivers State Government with support from PEPFAR through US Centers for Disease Control and Prevention (CDC). The two mentor mothers at OCH work with the PMTCT team to send out reminders for quarterly meetings. At these meetings, the pregnant women receive practical knowledge from doctors, nurses and mentor mothers who have experienced the same, about HIV and how to prevent their children and family from getting infected. The goal of the PMTCT support group meetings at OCH is working together to enable members attain viral suppression and live healthy lives.

Support group meetings at Obio have been on since 2011 and the hospital facilitates them by providing refreshments, transport fare for the participants at every meeting and by organising end-of-year parties and distributing gifts. Aderonke says the meetings used to be monthly but because funds are scarce, it had to become quarterly. She says the support groups are just an additional way to keep clients engaged and the groups exist beyond the meetings though as friendship and even business partnerships are formed as members are encouraged to exchange phone numbers and patronise each other’s businesses.
At the meetings, HIV positive mothers, old and new, share the stories of their journeys, how they disclosed their status to their partners, their challenges and commonalities, and the lessons they have learned to remind each other that there is hope, together.
Beyond Obio Cottage Hospital — Community Case Finding
With HIV-associated stigma and the time it takes for a HIV-positive person to become symptomatic, it is important to work to find HIV positive pregnant women who may need this support but are not aware of or willing to visit the antenatal clinics.
Obio Cottage Hospital’s PMTCT team conducts occasional community outreach visits to test, counsel and identify HIV positive pregnant women in the community and refer them to the clinic. They are then able to benefit from all the same services as those already registered in the facility.
The PMTCT officer said that out of over 800 babies in the program only 2 have tested positive. One came with a high viral load from another facility and the other simply did not take her medications as prescribed because of her religious beliefs. The clinic now records a 99% success rate in preventing mother to child transmission of HIV. Dunni and Tari have joined the Obio community health insurance scheme, they now attend antenatal at OCH and are mentor mothers to other clients under the PMTCT programme.
Obio Cottage Hospital and the success of its PMTCT program shows the sustainable impact of a 10-year public-private people partnership between SPDC and its Joint Venture Partners who provided advisory and technical oversights including financial support.
Dr Akin Fajola, Regional Community Health Manager at Shell Nigeria said that the PMTCT program has helped to change attitudes, perceptions and the initial stigma towards PLWAs by the community. He added that one of the net benefits has been the off shoot PMTCT support group which has taken on a life of its own from 5 women in 2012 to over 150 today and from one facility to other SPDC – JV supported facilities. This has improved their quality of life and has become a support system for social and economic empowerment.

Some of the limitations the program faces are generally linked to limited funds. The support group meetings which should ideally be at least once a month but are now quarterly because of funds. They would like to have more community outreaches to get more HIV positive women into supportive care but again funds are a challenge.
Leaning more on the use of mobile phones and technology to incentivise and encourage continued participation in the PMTCT program is one cheaper way that the program can employ, as this study shows.
The religious beliefs of some clients can also be a barrier. Isoken (not real name), a PMTCT client at OCH experienced a relapse in her health because she attended a church where she was told HIV is not real. She stopped taking her drugs for a month, became critically ill and had to be admitted into intensive care. “I nearly lost my life and my husband ran away because my look and colour changed so much” She lamented. Thankfully she is now healthy and says she would never listen to any cleric who tries to stop her taking her medication.

Adapting for COVID-19
Most businesses and facilities are adapting to continue to deliver safe services during the COVID-19 pandemic and this is also evident at the PMTCT clinic at OCH. The hospital has initiated formations and patterns for patient movement to control crowds. Antenatal clinics and classes are now staggered to morning, afternoon and evening sessions. To reduce non-essential hospital visits for antiretroviral therapy, more ARV medicines are given so that clients do not have to come back as often. Scheduling and synchronising are done so that most clients do not need to visit the hospital more times than necessary.
As important as these measures are to prevent the spread of the pandemic, Aderonke fears that they may be affecting their test-all policy and as such the number of HIV positive mothers they can find and treat. Already the number of HIV positive cases from the GOPD have dropped from an average of 20–30 per month to 10 in April. As much as the team wants to see HIV positive cases drop, they do not want it to be because people are not getting tested and treated.
PMTCT services should be offered before conception, and throughout pregnancy, labour and breastfeeding. Facilities implementing PMTCT programs should strengthen their counselling. Care at PMTCT units should be patient-centred, compassionate and confidential. This is the Obio OCH model and it has shown incredible success for positive mothers. The challenge is to build on what exists to create a sustainable and adequately funded model that can be replicated across the country and elsewhere.



Excellent article. Kudos to the hard working staff of Obio Cottage Hospital, Port Harcourt.
This is a timely and powerful reminder that while COVID-19 is currently engaging our attention and rightly so, access to essential, high quality and affordable health services is a right and not a benefit and that Universal Health Coverage that ensures that “No is left behind” must be given an utmost priority by all WHO member nations. We must remember that disease conditions like TB, HIV/AIDS, Malaria, Lassa fever, NCDs etc are still very much with us with their attendant unacceptable high mortality and morbidity.
A global health crisis like COVID-19 and a strong health system are 2 sides of the same coin. We need a robust and resilient health system that can withstand the shocks brought on by a major public health challenge. We have an opportunity in this crisis to step up and do the right thing for our people.
Can we see that?
Completely agree. The pandemic has shown that epidemic preparedness is not a one-off or one-disease issue but needs to be continuous and consistent. Clearly, global health security help achieve universal health coverage when the whole system is ready to handle epidemics without other existing health services suffering. So yes, our local, state and federal governments in Nigeria have a unique chance with all the renewed focus on the health sector to strengthen our health systems as a whole. As this starts to happen, we would document it.