By Dara Ajala-Damisa and Kemisola Agbaoye (Lead Writers)
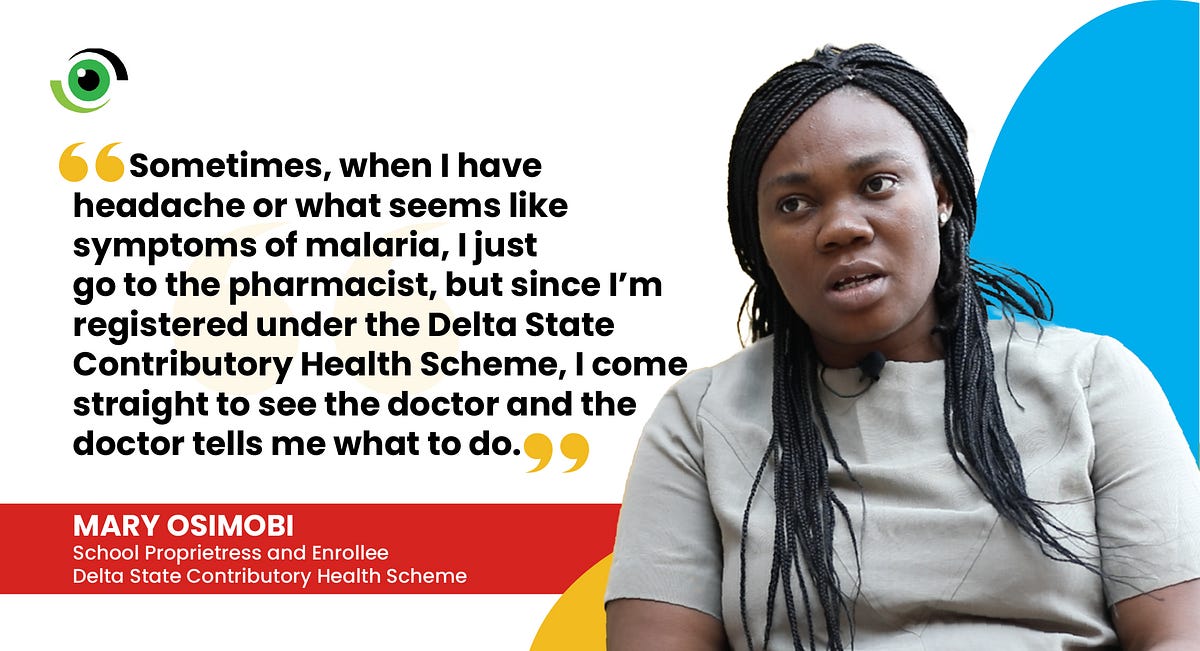
For reasons ranging from lack of funds and conflicting needs, to long wait times and convoluted registration processes, the average Nigerian would rather self-medicate or go to the neighbourhood pharmacy or chemist when they feel unwell, than go to a doctor.
Very few Nigerians can afford the services of private hospitals, and even fewer have health insurance. This means that when medical emergencies arise, they end up paying out of pocket. Available data has shown that in 2016, out-of-pocket expenditure for health in Nigeria accounted for up to 7.7billion naira. These factors can have a negative impact on the health seeking behaviours of the populace, especially women and children.
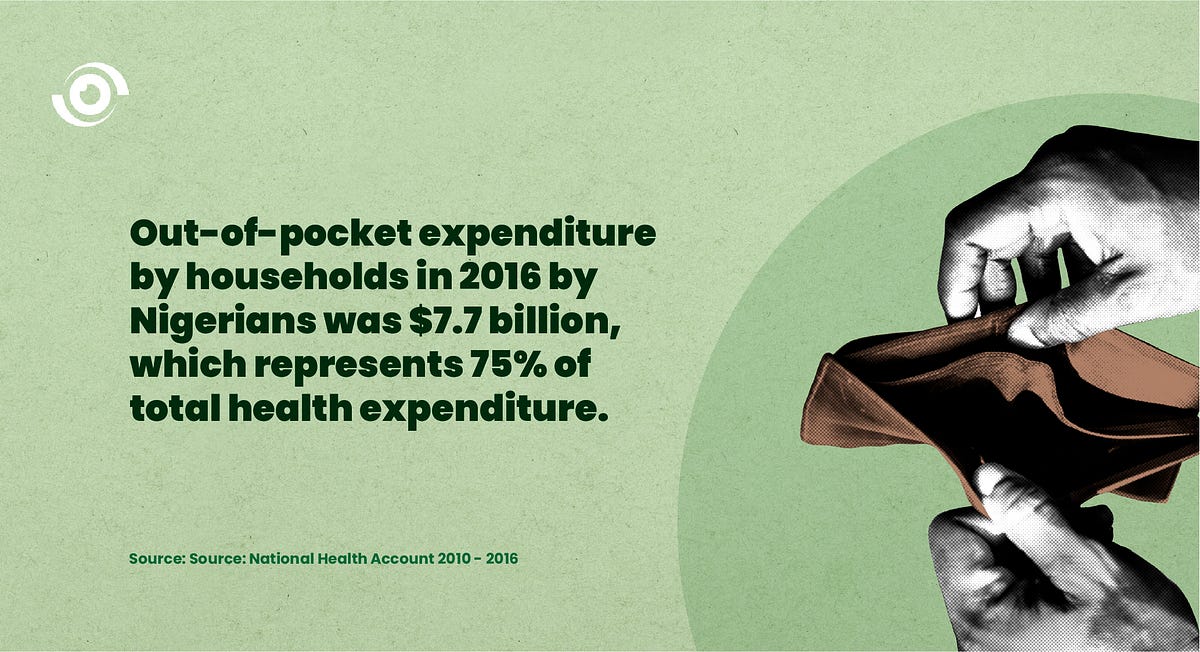
According to the World Bank, Universal health coverage (UHC) aims to ensure that all individuals and communities have access to the healthcare they need without suffering financial hardship. One of the targets of Sustainable Development Goal (SDG) three (3.8) aims to “achieve universal health coverage, including financial risk protection, access to quality essential health care services, and access to safe, effective, quality, and affordable essential medicines and vaccines for all”. In addition, SDG1, aiming to “end poverty in all its forms everywhere” could be in peril without UHC, as almost 90 million people are impoverished by health expenses every year. In Nigeria, the urgency to achieve Universal Health Coverage is even more pronounced with 76.6% of the country’s health expenditure coming from out-of-pocket expenses. This is in a country where almost 83million people live below the poverty line, meaning that a large proportion of these health expenses end up throwing Nigerians deeper into poverty.
The National Health Insurance Scheme (NHIS) in Nigeria was established in May 1999, with the vision of, “achieving financial access to quality healthcare for all Nigerians”. In part, the act states that the purpose of the scheme is to “… provide health insurance, which shall entitle insured persons and their dependants the benefit of prescribed good quality and cost-effective health services…” The NHIS was created as a tool for achieving UHC, but thus far only 5% of the population (mostly in the formal sector) has been enrolled since its establishment. Currently going through repeal and re-enactment to rebrand as the National Health Insurance Agency, the proposed NHIA bill awaiting assent by the President focuses more on regulation as well as improved funding for vulnerable groups. To fast-track UHC achievement, the 2014 National Health Act provided legislative backing for states to establish their own contributory health insurance schemes. As of January 2020, 34 states and the FCT have signed social health insurance schemes into law, with states such as Delta, Kaduna, Kano, Plateau, Lagos, Oyo, Yobe, etc. making significant progress in enrolment of lives.
The Delta State Contributory Health Scheme
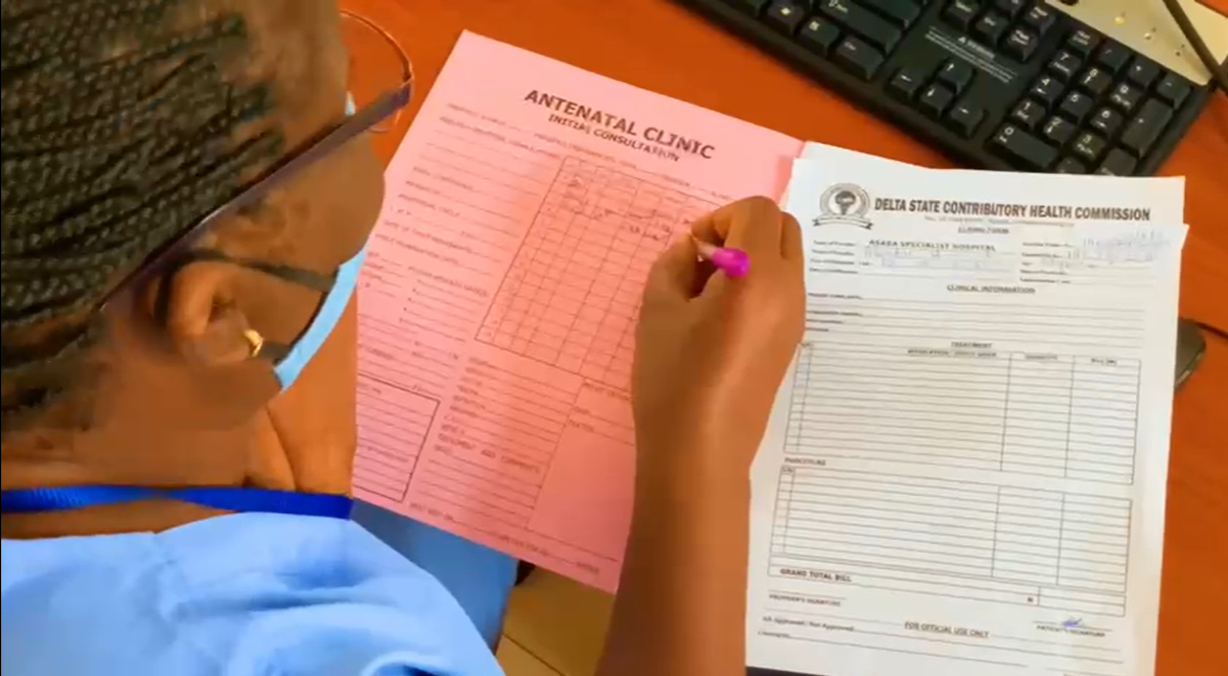
The Delta State Contributory Health Scheme was established in 2017 to provide quality and affordable health care to all residents of Delta state. The scheme is managed by the Delta State Contributory Health Commission (DSCHC).
The scheme has enrolled over 1 million lives since its establishment. Enrolees pay a yearly premium applicable to the plan they choose which allows them to access quality healthcare at accredited facilities under the scheme at no additional cost.
The scheme offers four plans which are designed to cater to all residents of Delta state, irrespective of social or financial status. The plan for the formal sector caters to civil servants and employees in the organised private sector; for the plan catering for individuals in the informal sector, such as artisans, traders, and day labourers, enrolees pay a flat rate of NGN7,000 per individual every year; under the Equity Plan, the State Government pays the premium for vulnerable citizens like pregnant women and children under 5; and to get on the Private plan, enrolees pay a little extra to enjoy more services.
Comrade Bolu Martin, Director of Administration and Human Resources at the DSCHC, gave some insight into the inner workings of the scheme and the progress it has made so far. “The scheme is designed to improve the health care system, and to enhance the capacity of health care facilities so that people can get quality healthcare. The hospitals are paid in two ways, one of which is what we call capitation. Every month, a stipulated amount of money is paid to the hospitals, regardless of whether patients come in or not. This means there are always funds available to the hospital when the need for treatment does arise. Healthcare facilities can also use funds from this pool to improve their facilities.”

The Equity plan of the scheme plays a major role in increasing positive maternal and child health outcomes, one of the goals of the scheme. The individuals who fall into this category are pregnant women, children under the age of 5, men and women over the age of 65, and physically or mentally challenged persons. The scheme leveraged the State’s already existing free maternal and under 5 program to achieve this. The State Government ensures sustainability of the Equity Plan through investment partnerships with the Bank of Industry (BOI) and setting aside a percentage of the budget to fund the plan with contributions from donor agencies.
What are the factors responsible for these encouraging numbers?
Delta state has enrolled about one million of its over 5 million citizens, which is around 17 percent of its citizens. Obasa Lilian Chineyeye, Health Maintenance Organisation (HMO) Coordinator for Good Christian Medical Centre, Asaba, reflecting on the impact of the scheme stated that the number of enrolees who chose Good Medical Christian Centre as their primary facility increased from 5 in 2017 to 3644 in 2021.

One of the factors responsible for the increased enrolment of people from Delta state is continuous community advocacy and engagement. The DSCHC meets with town unions, community elders and stakeholders, as well as political groups to sensitise them on the benefits of enrolling in the Scheme. A further powerful tool in getting buy-in is testimonials from beneficiaries. Mr Tony Izuka, a civil servant, was reluctant to sign up because he was afraid that the healthcare facility would be sub-standard. He was pleasantly surprised to discover that this was not the case, as he received excellent care. Mr Izuka now encourages other civil servants to sign onto the state health insurance scheme. The registration, claims, payment and reporting process is operated by Artificial Intelligence (AI), which has made user interface easier and eliminated the element of human error. The registration process is end-to-end encrypted to ensure enrolee data privacy. The scheme was named a “contributory health scheme” with the term “insurance” eliminated, to overcome the bias associated with insurance schemes in the region.
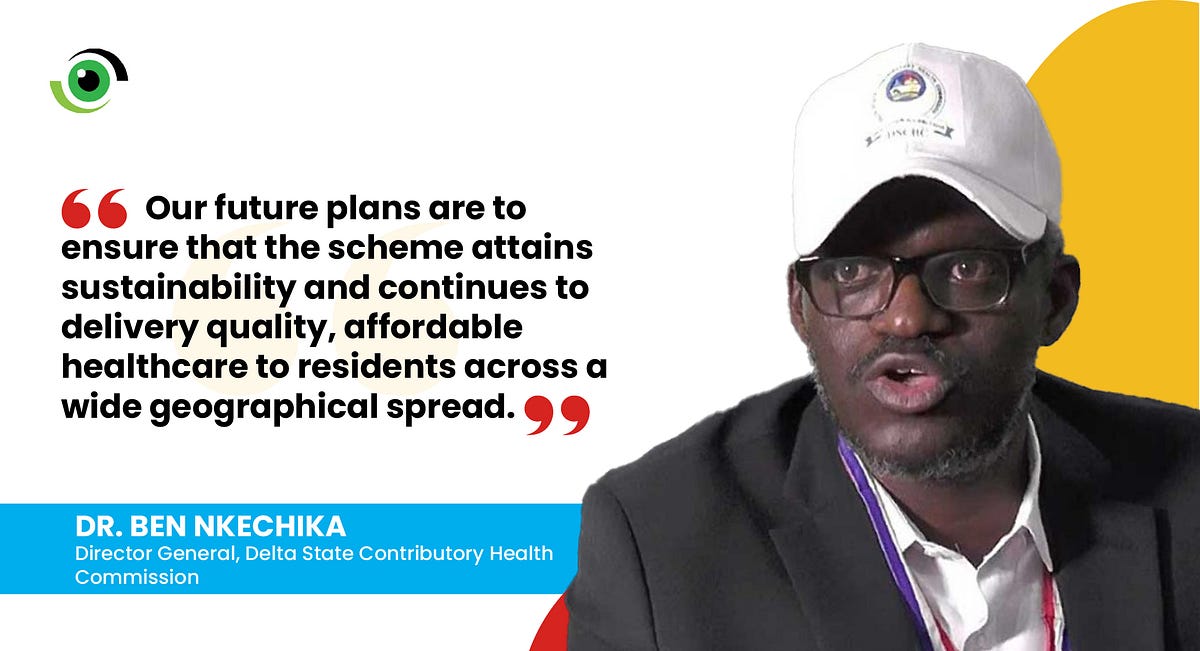
To ensure effective coordination, the Director General of the Commission, Dr Ben Nkechika, set up multiple teams, including technical compliance, process monitoring and technical integration teams to oversee the process and course correct as they go. These teams are all locally staffed, and the Scheme is run with no development aid or support, further promoting ownership.
Clinton Ekaeze, Technical Assistant to the DG of the Commission pointed out that access to finance programmes has made it possible for healthcare facilities to be fully operational 24–7 in riverine communities, where previously this was not possible. Mr Ekaeze also noted that partnerships with pharmaceutical companies has made access to quality medicines easier. Ekaeze and Martin both agree that developing tailor-made solutions to solve unique state problems, rather than just copying what others have done has greatly contributed to the budding success of the Scheme.
The impact of the DSCHC underscores the critical role of Public Private Partnerships (PPP) in delivering healthcare. A good example of the PPP landscape in Delta State is the Medical Credit Fund made possible in part by the contribution of partners including PharmAccess, a technical advisor that helped to increase access to finance programmes, supported by Bank of Industry.
What needs work?
While ensuring access to quality health care is one of the foremost goals of the Scheme, it has been a constant struggle to achieve this, as the actual running of the health facilities is not completely under the influence of the Scheme. For example, according to Dr. Owuigho Oghene, strike actions by health personnel make it impossible for beneficiaries to access 24/7 quality health services, despite the payment of capitations to the health facilities. According to Comrade Bulu Martin, there have also been instances where beneficiaries have had to pay for certain services such as blood transfusion even though the insurance premium covers it, due to the duplicity of health facility workers.
Health worker and health facility collaboration and cooperation continue to be a challenge that needs to be addressed to make full progress towards Universal Health Coverage. In addition, key stakeholders at the DSCHC indicate that though some progress has been made in enrolling the informal sector, this has not happened as quickly as is needed to ensure more residents have access to quality, affordable healthcare.
While the journey so far has not been without its challenges, the DSCHC is proud of the progress of the Scheme thus far and is primed to achieve even more. According to Dr Ben Nkechika, the state is looking to achieving an additional 20% coverage within the next four years.
Of the 34 states that have passed health insurance laws, different levels of progress have been seen as regards making progress towards Universal Health Coverage. As we observe World UHC Day in a few days, we encourage states to continue to collaborate and learn from each other to improve access to care.